- Home
- Features
- Business
- Active
- Sports
- Shop
Top Insights
PREFER recommendations for patient preference studies

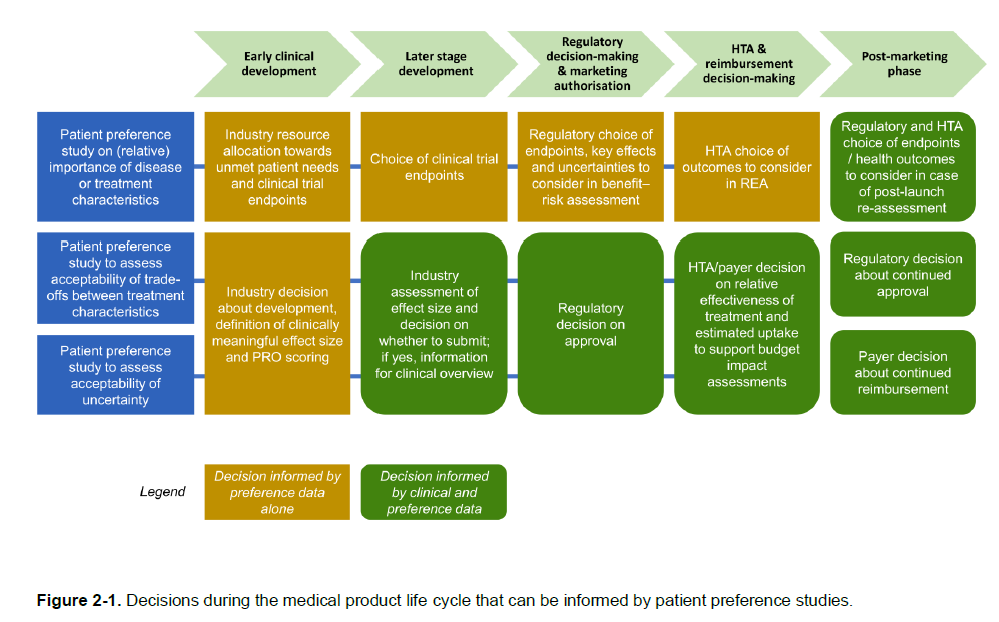
Patient preferences should be the most important part of health care decisionmaking. However, third parties often make decisions for patients. Physicians make decisions for patients due to asymmetric information (i.e., physicians are experts; patients typically are not). Payers make decisions for patients since–in most developed countries–third-party payment cover most of the cost. Moreover, in some cases caregivers may also make decisions. Thus, while in most markets the consumer makes the decision and the purchase based on their own preferences, in health care patient preferences are not always central to the decision-making process.
The IMI PREFER initiative aimed to provide guidance on how patient preferences can be incorporated into decisionmaking. Their nearly 300 page report has a variety of recommendations for incorporating patient preferences. Here are some key takeaways:
When to incorporate patient preferences?
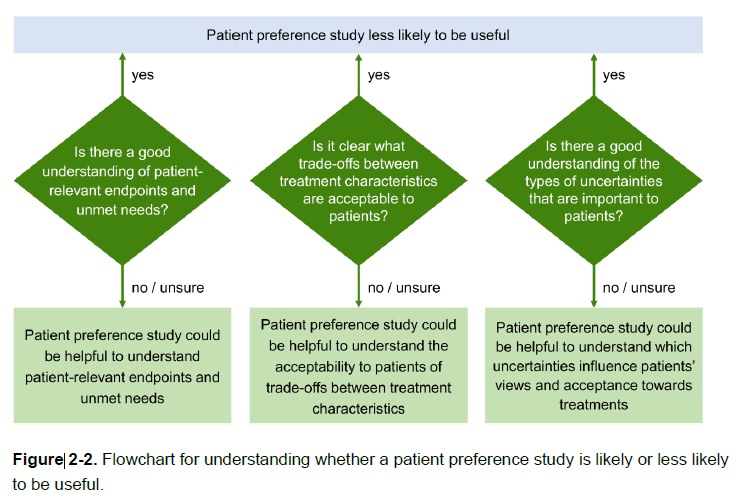
Are there cases where patient preferences are less likely to be useful?
Yes, If relevant endpoints, tradeoffs are well known and there are few uncertainties, then the value of conducting a patient preference survey could be less.
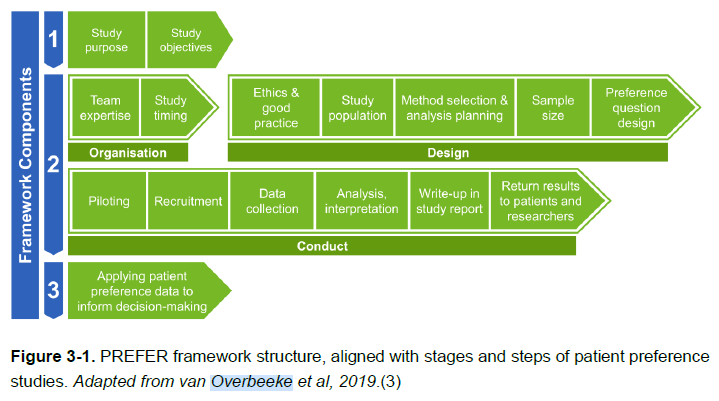
What are the steps needed to conduct a patient preference study?
The PREFER approach draws from Overbeeke et al. 2019 and describes the steps/phases as shown below.
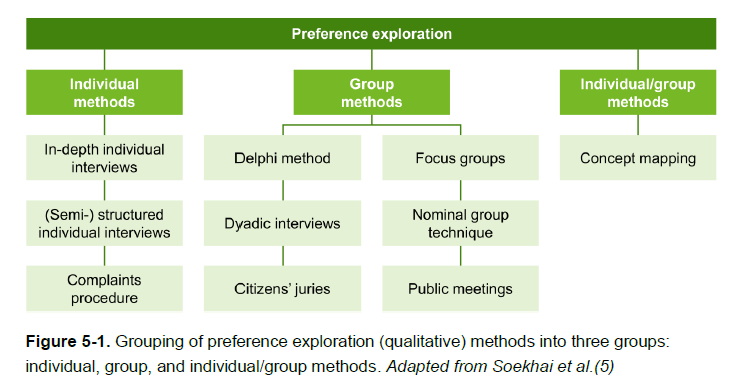
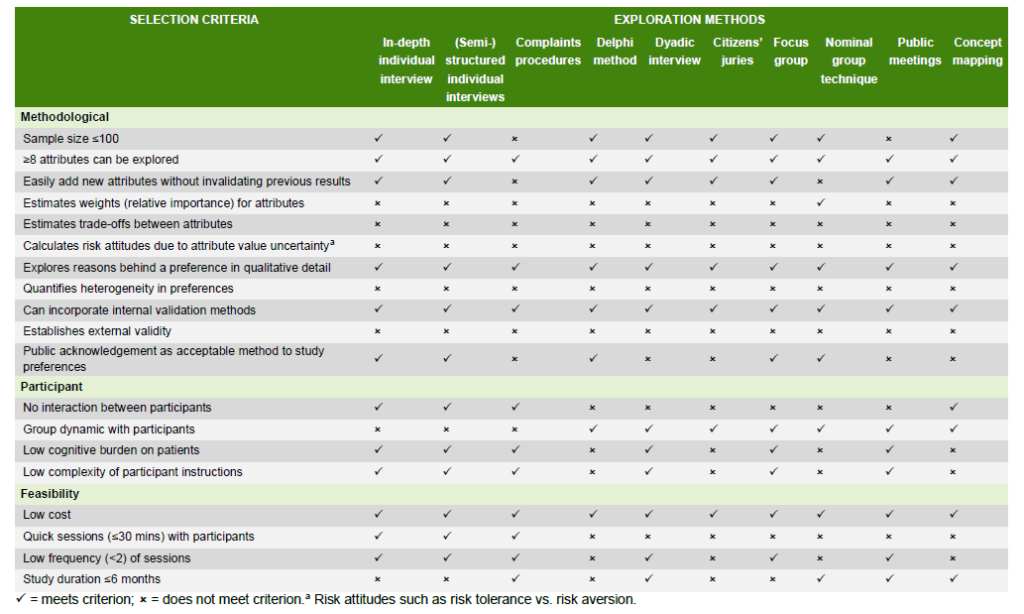
What is preference exploration and what methodologies are available to conduct it?
In-depth exploration of the patient perspective regarding their disease, treatments, and the
importance of outcomes or attributes is often conducted using qualitative methods. These qualitative methods are often best-suited for early phases in the medical product life cycle. Relevant methods include:
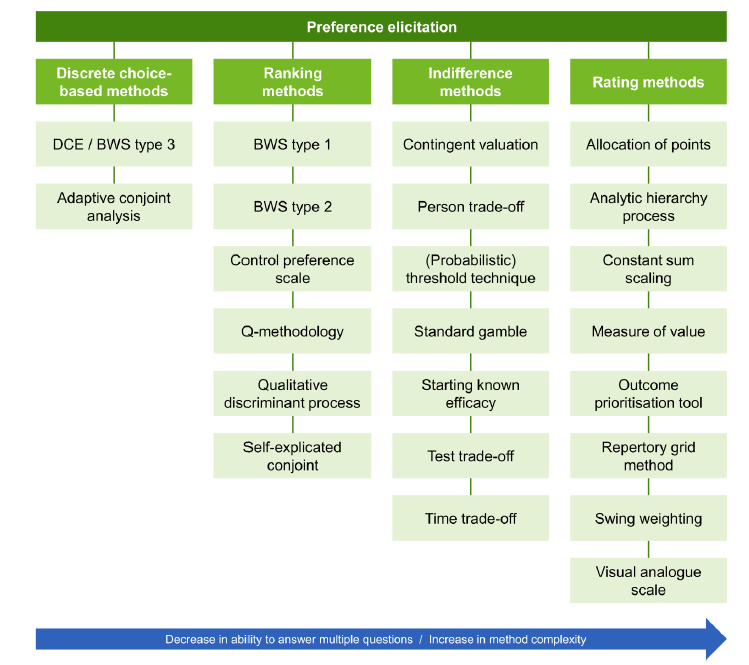
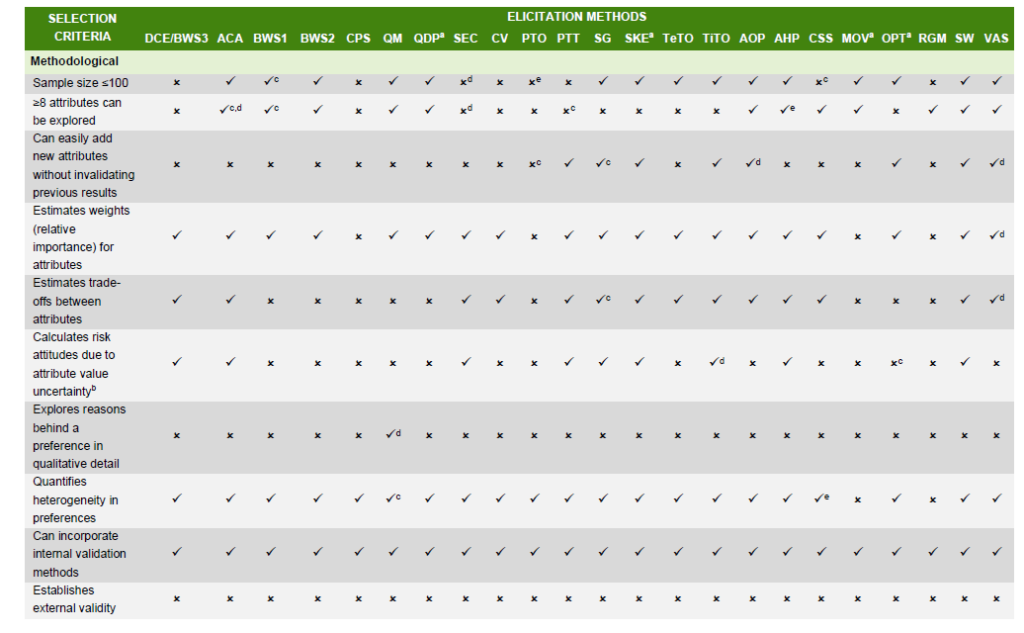
How can I quantify these preferences?
The PREFER methodology lists different types of methods from Soekhai et al. (2019). The performance matrix to evaluate these quantitative elicitation methods was adapted from Whichello et al, 2020.
There is much more great information in the recommendations report here.
Recent Posts
Categories
Related Articles
This year’s ViVE conference was full of announcements — from acquisitions to...
ByglobalreutersFebruary 21, 2025PEPFAR, the U.S. global HIV/AIDS program, is - for the first time...
ByglobalreutersFebruary 20, 2025In Feedspot’s 2025 rankings, Healthcare Economist was once again ranked in the...
ByglobalreutersFebruary 20, 2025






Leave a comment